Direct Correlation Between Arthritis and Oral Health


Meet the Author: Sara Juliano, RDH
I have been a registered dental hygienist for over a decade. I have had the pleasure of working with amazing patients and educating them on their oral health throughout my career. Recently, I made the conscious decision to branch out within the dental field, choosing to maintain my dental hygiene license, and become a dental educator. With a passion for oral and systemic health, I have seen clinically the direct impact systemic health can have on oral health. I will be extending my knowledge outside of the dental chair into the world and make an impact on the lives of others.
As a Registered Dental Hygienist for over a decade, I have had many patients that suffer with this widespread, chronic auto-immune disease come into my dental office. As oral health care providers, it is our job to provide those who suffer from Arthritis an understanding of the correlation between their suppressed systemic health and the impact it has on their oral health.
What is Arthritis?
Over one third of the population suffers from arthritis. Arthritis is a disease that affects the joints in the body by attacking and breaking down the synovial fluid that gives joints free range of motion. This inflammation degenerates the tendons, ligaments and bones causing extreme pain. There is currently no cure for arthritis.
Our bodies create proteins called Cytokines. Cytokines, in a healthy state, reduce inflammation in the body. When the body recognizes these proteins as foreign, they “self-attack “and the reverse takes place causing an increase in inflammation. These cytokines release toxins that breakdown the joints, ligaments and tendons and eventually the surrounding bones that support the joints.

If you’d like to learn more about Rheumatoid Arthritis and its connection to periodontal diseases, check out the first episode the Teeth Chatters podcast!
Arthritis and Oral Diseases
There have been case studies that have proven there is a strong correlation between Arthritis and oral diseases. Scientists have found the bacterium P. Gingivalis in synovial fluid that surrounds joints throughout the body. P. Gingivalis is predominantly a bacterium in the oral cavity. If the bacterium is not effectively removed by daily mechanical brushing, routine flossing, and using antimicrobial oral rinses to reduce plaque formation of P. Gingivalis, then the bacterium will migrate below the gumline. This releases toxins, and ultimately destroys the ligaments, collagen connective fibers, and bone that support the teeth, resulting in a disease state in the oral cavity called Periodontal disease.
What is Periodontal Disease?
Periodontal disease is a destructive inflammatory disease of the dental supporting tissues and structures (Connective tissue, ligaments, and erosion of the bone surrounding the teeth). In clinical studies of periodontal disease, there are high levels of inflammatory infiltration of the bacterium P. Gingivalis. Once this bacterium migrates below the gumline and goes subgingivally, it then will release toxins that will destroy the tissue and bone and result in irreversible loss of tissue attachment and bone.
In the early to moderate stages of periodontal disease there usually are no symptoms or pain associated with the disease. Therefore, it is vitally important to have routine dental exams and cleanings so your dentist, as well as your dental hygienist, can do thorough periodontal probing measurements to evaluate if there is any sign of bone loss and attachment that supports and surround the teeth. Periodontal disease can be very specific to a localized area or can become generalized. Thorough debridement of supra and subgingival plaque and tartar is necessary to significantly reduce the bacterium in the mouth so that further destruction to the mouth and other areas of the body will be minimized.
Periodontal Disease & Arthritis
Periodontal disease is more common among people suffering from Arthritis and other systemic health issues. It is vital to have optimal oral health when diagnosed with Arthritis. Having good oral hygiene decreases plaque formation in the oral cavity and reduce bacterial migration to the rest the body. In the case of Arthritis, it will significantly reduce inflammation around the joints and reduce the destruction of the ligament, tendons, connective fibers and bone.
Periodontal disease and Arthritis are the most prevalent inflammatory diseases of the body known today. Plaque reduction to the rest of the body starts with good oral hygiene.
Dry Mouth & Arthritis
Additionally, most people that have Arthritis are on several medications and oral steroids to help alleviate the pain and inflammation in their bodies. Dry mouth also known as Xerostomia, is the main side effect and most common side effect of polypharmacy. Dry mouth can create issues in the oral cavity such as pH changes that will create acidic environments for cavity formation, plaque accumulation, dry throat, trouble swallowing, altered taste in the mouth, thick ropey saliva, and burning sensation. Having a moist oral cavity is essential for everyone especially those of us suffering from systemic health issues because the body is already in an immunocompromised state.
A low salivary flow will cause plaque to stick to the teeth, tongue, and surrounding oral tissue. When the normal salivary function is absent in the mouth, proper removal or oral clearance of food debris is very low, this allows the plaque and bacterial biofilm time to adhere to the oral cavity. Dry mouth increases the plaque accumulation which results in an increase of bacterium (P. Gingivalis) that causes inflammation in the periodontium (the bone that supports the teeth) and the surrounding bone and joints in those suffering from Arthritis.
Oral Care & Arthritis
It is important for people suffering from Arthritis to have routine dental checkups and cleanings and to stay on top of their oral health. Periodontal disease is progressive and can be stabilized in the diseased state and maintained with proper oral health, to prevent further degradation of the bone and remain stable. Proper oral care includes:
- Brushing your teeth properly at least twice a day
- Using a tongue scraper
- Treating flossing as important as brushing
- Using mouthwash

What is Lubricity?
Lubricity is an odorless, flavorless, and colorless spray that is perfect for people who are overly sensitive to taste. Our Dry Mouth Spray also has Zero Calories, NO Gluten, NO Alcohol, NO Sugar, and is Vegan-Friendly!
Lubricity Dry Mouth Spray has 5 simple ingredients: Hyaluronic Acid, Xylitol, Sodium Benzoate, Potassium Sorbate, and Purified Water. This simple formula is clinically proven to alleviate your dry mouth symptoms for up to 4 hours.
How to use Lubricity?
Lubricity Dry Mouth Spray comes in a convenient 0.5 oz and 2oz spray bottle. Simply point and spray 3-5 times per use. When used as directed, Lubricity provides up to 4 hours of relief from dry mouth symptoms.
For best results, we recommend using Lubricity Dry Mouth Spray as follows:
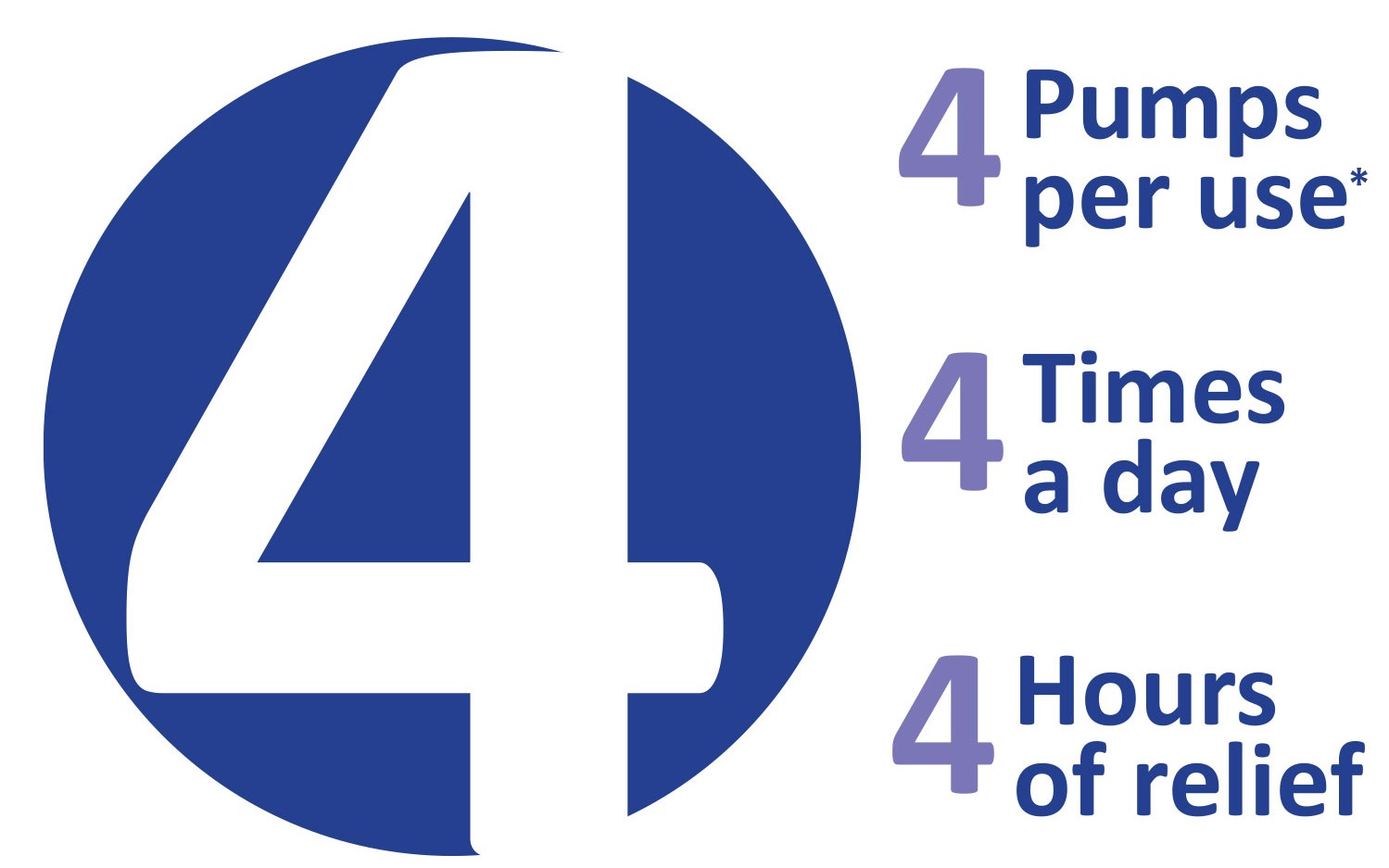
Use Lubricity after a meal and before bed. If needed, Lubricity can be used more than 4 times per day.
*Some may need 3-5 pumps per use, as the bottle needs to be primed upon opening. Relief from symptoms begins immediately. Maximum effectiveness is achieved after 72 hours of continued use.
Important: If you are pregnant or breastfeeding, please consult your physician before using Lubricity. DO not use Lubricity if you are taking any medications that are contraindicated with the product. Please consult with your physician if you have any concerns regarding the use of this product. Keep out of reach of children.





